What is degenerative disc disease?
Degenerative disc disease (DDD) is a chronic and progressive condition that is characterized by inflammation and breakdown of tissue within the intervertebral disc. It is a major cause of chronic low back pain, which is the leading cause of disability worldwide.
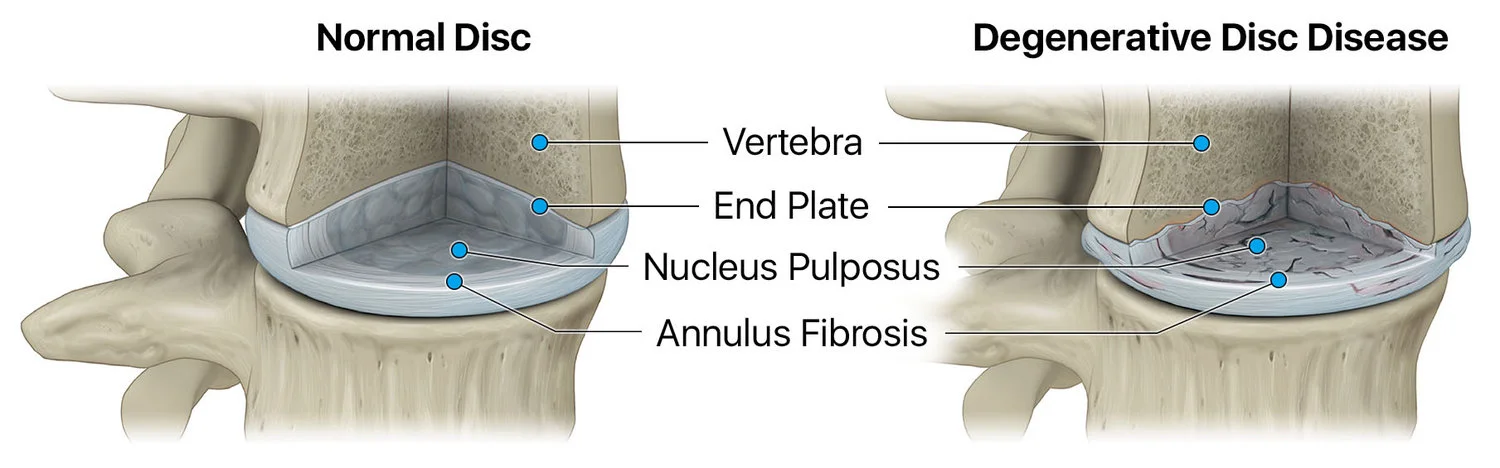
When the intervertebral disc becomes inflamed and loses its structure, the disc tissue becomes rigid and weakened, and begins to collapse. This can result in pressure being applied to the surrounding nerves in the spinal column, causing pain and loss of function.
Pain is most commonly felt or made worse by movements such as sitting, bending, lifting or twisting.
What is the intervertebral disc?
The intervertebral disc is located between the vertebral bones in the spine and acts like a pillow to cushion and evenly distribute pressure across the vertebrae. Each disc is comprised of an outer fibrous ring, the annulus fibrosis, which surrounds an inner gel-like center, called the nucleus pulposus.
How is degenerative disc disease diagnosed?
To help determine if you have degenerative disc disease, a physician will assess your medical history, conduct a physical exam and, in many cases, order diagnostic imaging, such as an x-ray, CT scan or MRI scan.
How is degenerative disc disease currently treated?
In the earlier stages of DDD, current treatment options include physical rehabilitation programs and pain management approaches that are typically not intended for long-term use. Opioids, epidural steroid injections and radiofrequency ablation are a few examples of these.
In the more advanced stages, surgical intervention may be required to remove the patient’s painful disc(s), fuse two or more vertebral bones together, and/or replace bone or tissue altogether.
While these options may offer temporary pain relief, they do not directly address the root cause of the pain: the degenerated disc.